Human immunodeficiency virus (HIV) is a retrovirus that infects and gradually destroys the immune system’s CD4+ T cells, leading to acquired immunodeficiency syndrome (AIDS). While antiretroviral therapy (ART) has successfully suppressed viral replication, it cannot eliminate the virus from the body entirely. HIV persistence in long-lived reservoirs, such as latently infected CD4+ T cells, poses a significant challenge to finding a cure for HIV/AIDS. One promising approach to eliminating HIV reservoirs is through immune activation. In this essay, we will discuss the mechanisms of immune activation and their role in HIV persistence, as well as the potential therapeutic targets for immune activation.
How persistent is HIV?
The mutation rate of HIV is high, which permits it to evade the immune system and develop resistance to antiretroviral therapy (ART) over time.
One of the reasons HIV is persistent is that it can establish a latent or dormant infection in CD4 T cells. When HIV infects a CD4 T cell, it can integrate its genetic material into its DNA, creating a reservoir of infected cells that are not actively producing virus particles. The immune system or ART does not detect these cells and can persist for years, even decades, in the body.
HIV can also persist through the phenomenon of viral rebound. Even when ART suppresses viral replication to undetectable levels, there may still be small amounts of the virus in the body. If ART is discontinued, these residual virus particles can rapidly replicate, leading to a rebound in viral load.
Moreover, HIV can persist in other reservoirs, such as the brain, lymph nodes, and gut-associated lymphoid tissue. These reservoirs are difficult to access and may require different treatment approaches to eliminate the virus.
What is Immune activation?
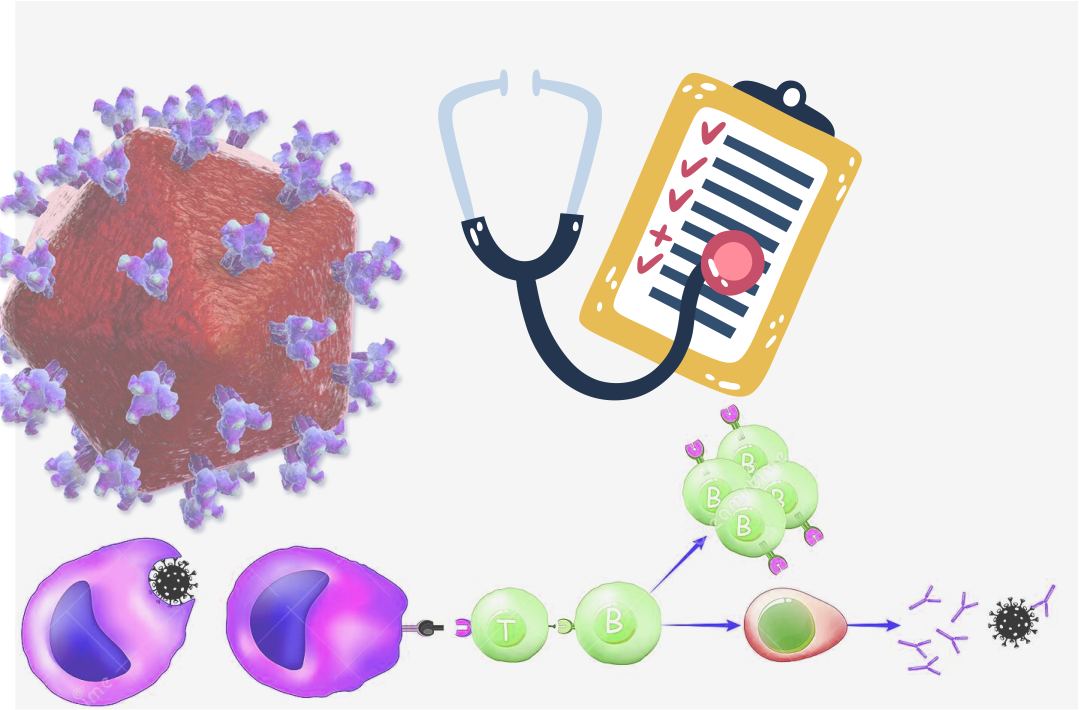
Immune activation is a process by which the immune system is stimulated to respond to infectious agents or other foreign substances. It involves activating immune cells, such as T cells, B cells, and natural killer cells, and releasing cytokines and chemokines. Immune activation is crucial in controlling HIV infection by limiting viral replication and promoting the clearance of infected cells. However, chronic immune activation can also harm the immune system, leading to immune exhaustion, inflammation, and tissue damage.
In the context of HIV infection, immune activation is a double-edged sword. On the one hand, it is important to control viral replication and prevent disease progression. However, on the other hand, chronic immune activation contributes to HIV persistence by creating an environment that supports viral replication and inhibits the clearance of infected cells. This chronic immune activation is thought to be caused by the persistent presence of viral antigens and the dysregulation of immune cells, leading to immune dysfunction.
How is immune activation useful in eliminating HIV?
One potential therapeutic approach to eliminate HIV reservoirs is to use immune activation to stimulate the clearance of infected cells. Immune activation can be achieved through several mechanisms, including therapeutic vaccines, immune checkpoint inhibitors, and Toll-like receptor (TLR) agonists. Therapeutic vaccines are designed to boost the immune response to HIV antigens, thereby enhancing the clearance of infected cells. Immune checkpoint inhibitors, such as anti-PD-1 and anti-CTLA-4 antibodies, can release the brakes on the immune system, allowing it to mount a more robust response to the virus. Finally, TLR agonists can activate innate immune cells, such as dendritic cells and macrophages, to produce cytokines and chemokines that promote the clearance of infected cells.
While immune activation shows promise as a potential therapeutic approach to eliminate HIV reservoirs, there are also potential risks associated with this strategy. Chronic immune activation can lead to immune exhaustion and inflammation, which can exacerbate HIV disease progression and increase the risk of non-AIDS-related complications. Furthermore, immune activation may also activate latent HIV reservoirs, leading to viral rebound and the re-establishment of HIV infection.
Conclusion
In conclusion, immune activation is a promising therapeutic approach to eliminating HIV reservoirs and achieving a cure for HIV/AIDS. However, the mechanisms of immune activation and their role in HIV persistence are complex, and further research is needed to understand the risks and benefits of this strategy fully. Nevertheless, the potential therapeutic targets for immune activation, including therapeutic vaccines, immune checkpoint inhibitors, and TLR agonists, offer hope for a cure for HIV/AIDS in the future.